Miðað við tölur frá Alþjóðaheilbrigðismálastofnuninni, sem þegar þetta svar er skrifað ná til 31. ágúst 2025, hafa yfir 778 milljón tilfelli COVID-19 greinst á heimsvísu frá upphafi talningar. Fjöldi áætlaðra dauðsfalla er að minnsta kosti 7 milljónir og fjöldi innlagna er margfalt meiri. Rétt er að taka fram að tölurnar eru vanmetnar enda skráningum víða ábótavant.
- Staðfest tilfelli COVID-19 eru ávallt vanmat á umfangi sjúkdómsins í samfélagi, enda eru mörg tilfelli aldrei formlega greind.
- Skilgreiningar á COVID-19 sem dánarorsök eru breytilegar eftir tíma og stað. Áreiðanleg gögn sýna að fyrir tíma ómíkron-afbrigðisins var yfirgnæfandi meirihluti skráðra „COVID-19-dauðsfalla“ sannarlega vegna sjúkdómsins. Með tilkomu ómíkron-afbrigðisins hefur þetta hlutfall minnkað, en áfram eru flest dauðsföll sem skráð eru vegna COVID-19 sannarlega vegna sjúkdómsins.
- Vaxandi vitundarvakning er um að mörg dauðsföll sem áður voru ekki tengd við COVID-19 megi rekja til sýkingarinnar; þar má nefna heilablóðföll, hjartaáföll og aðra sjúkdóma.
- CFR horfir aðeins á dauðsföll en gefur ekki mynd af öðrum afleiðingum COVID-19.
- World Health Organization. (e.d.). COVID-19: Cases [gagnvirkt mælaborð]. https://data.who.int/dashboards/covid19/cases?n=c
- Salisu-Olatunji, S., Chudasama, o.fl. (2024). COVID-19-related morbidity and mortality in people with multiple long-term conditions: A systematic review and meta-analysis of over 4 million people. Journal of the Royal Society of Medicine, 117(10), 336-351. https://doi.org/10.1177/01410768241261507
- Bajema, K. L. o.fl. (2025). Severity and Long-Term Mortality of COVID-19, Influenza, and Respiratory Syncytial Virus. JAMA internal medicine, 185(3), 324–334. https://doi.org/10.1001/jamainternmed.2024.7452
- Lipski, D. o.fl. (2024). Assessment of COVID-19 risk factors of early and long-term mortality with prediction models of clinical and laboratory variables. BMC Infectious Diseases, 24(1), 685. https://doi.org/10.1186/s12879-024-09592-7 Böttcher, L., Xia, M., & Chou, T. (2020). Why case fatality ratios can be misleading: Individual- and population-based mortality estimates and factors influencing them. Physical Biology, 17(6), 065003. https://doi.org/10.1088/1478-3975/ab9e59
- National Institute on Aging. (2024, 24. október). Many deaths attributed to natural causes during the COVID-19 pandemic may have instead been due to the virus. https://www.nia.nih.gov/news/many-deaths-attributed-natural-causes-during-covid-19-pandemic-may-have-instead-been-due-virus
- Basoulis, D. o.fl. (2025). Deaths “due to” COVID-19 and deaths “with” COVID-19 during the Omicron variant surge, among hospitalized patients in seven tertiary-care hospitals, Athens, Greece. Scientific Reports, 15, 13728. https://doi.org/10.1038/s41598-025-98834-y
- Pifarré i Arolas, H. o.fl. (2021). Years of life lost to COVID-19 in 81 countries. Scientific Reports, 11(1), 3504. https://doi.org/10.1038/s41598-021-83040-3
- Huang, G. o.fl. (2023) The effect of the COVID-19 pandemic on life expectancy in 27 countries. Scientific Reports 13, 8911. https://doi.org/10.1038/s41598-023-35592-9
- Free, R. J. o.fl. (2025). Hospitalization for COVID-19 and risk factors for severe disease among children: 2022–2024. Pediatrics, 156(3), e2025072788. https://doi.org/10.1542/peds.2025-072788
- Peters, J. A. & Farhadloo, M. (2023). The effects of non-pharmaceutical interventions on COVID-19 cases, hospitalizations, and mortality: A systematic literature review and meta-analysis. AJPM Focus, 2(4), 100125. https://doi.org/10.1016/j.focus.2023.100125
- He, X. o.fl. (2024). Non-pharmaceutical interventions in containing COVID-19 pandemic after the roll-out of coronavirus vaccines: A systematic review. BMC public health, 24(1), 1524. https://doi.org/10.1186/s12889-024-18980-2
- Ahmed, F. o.fl. (2024). Systematic review of empiric studies on lockdowns, workplace closures, and other non-pharmaceutical interventions in non-healthcare workplaces during the initial year of the COVID-19 pandemic: Benefits and selected unintended consequences. BMC public health, 24(1), 884. https://doi.org/10.1186/s12889-024-18377-1
- Greenhalgh, T. o.fl. (2024). Masks and respirators for prevention of respiratory infections: A state of the science review. Clinical Microbiology Reviews, 37(2), e0012423. https://doi.org/10.1128/cmr.00124-23
- Boulos, L. o.fl. (2023). Effectiveness of face masks for reducing transmission of SARS-CoV-2: A rapid systematic review. Philosophical Transactions of the Royal Society A: Mathematical, Physical and Engineering Sciences, 381(2257), 20230133. https://doi.org/10.1098/rsta.2023.0133
- Zhou, F. o.fl. (2022). The association of intensity and duration of non-pharmacological interventions and implementation of vaccination with COVID-19 infection, death, and excess mortality: Natural experiment in 22 European countries. Journal of infection and public health, 15(5), 499–507. https://doi.org/10.1016/j.jiph.2022.03.011
- Murphy, C. o.fl. (2023). Effectiveness of social distancing measures and lockdowns for reducing transmission of COVID-19 in non-healthcare, community-based settings. Philosophical Transactions of the Royal Society A: Mathematical, Physical and Engineering Sciences, 381(2257), 20230132. https://doi.org/10.1098/rsta.2023.0132
- Maison, D. P. o.fl. (2025). COVID-19 clinical presentation, management, and epidemiology: A concise compendium. Frontiers in Public Health, 13:1498445. https://doi.org/10.3389/fpubh.2025.1498445
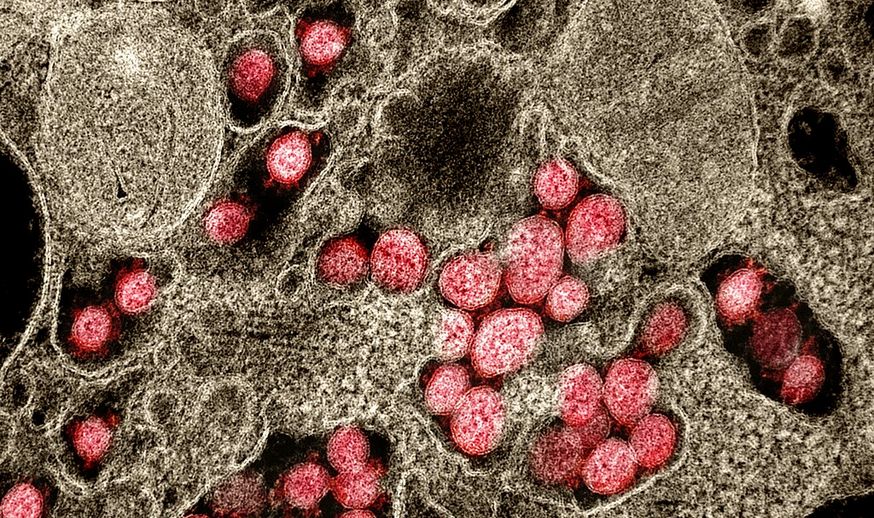
- Yfitlitsmynd: File:Novel Coronavirus SARS-CoV-2 (49597020718).jpg - Wikimedia Commons. (Sótt 25.11.2025). Myndin er birt undir CC-leyfi.
- File:COVID-19 pandemic. Chernivtsi, Ukraine.jpg - Wikimedia Commons. (Sótt 25.11.2025). Myndin er birt undir CC-leyfi.